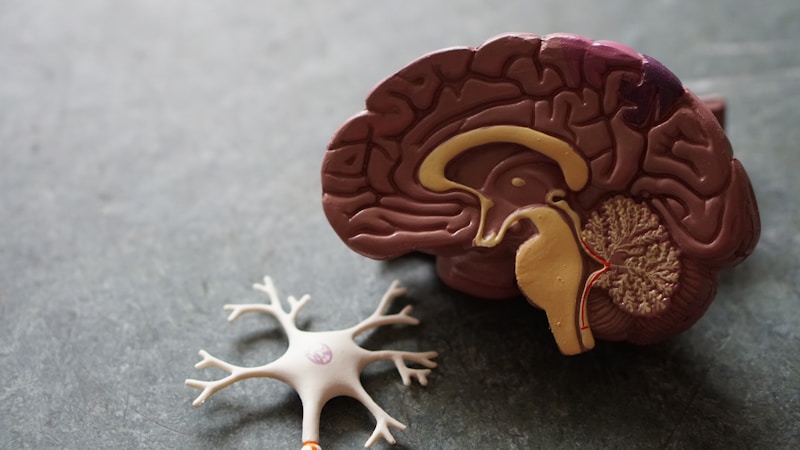
Post-Traumatic Stress Disorder (PTSD) is not a weakness or a choice. It is a real clinical condition, with well-documented neurobiological foundations, that occurs when the nervous system remains “stuck” in survival mode after a traumatic experience. Understanding PTSD is the first step toward effective treatment and recovery.
What Is PTSD?
PTSD (Post-Traumatic Stress Disorder) is a mental health condition that can develop after exposure to a traumatic event — an experience in which your life or physical integrity, or that of others, was threatened. According to DSM-5-TR (APA, 2022), PTSD involves four groups of symptoms that persist for more than one month and significantly affect functioning.
The Four Symptom Clusters
1. Re-experiencing (Intrusions)
Traumatic memories “invade” the present involuntarily and intensely:
- Flashbacks — You relive the event as if it were happening right now, with complete physical and emotional sensations
- Nightmares — Recurring dreams related to the trauma or with themes of threat
- Intense physiological reactions — Heart races, sweating, trembling upon contact with stimuli reminiscent of the event
- Emotional distress — Intense sadness, fear, or anger at reminders of the trauma
2. Avoidance
The constant effort to avoid anything reminiscent of the trauma:
- Avoiding thoughts, feelings, or discussions about the event
- Avoiding places, people, activities, or situations associated with the trauma
- Avoiding emotions (emotional numbness)
- Isolating from activities and people that were previously important
3. Cognitive and Mood Changes
Persistent changes in thinking and emotional state:
- Persistent negative beliefs (“The world is completely dangerous,” “I am irreparably broken”)
- Distorted guilt or shame related to the event
- Persistent negative emotions (fear, anger, guilt, shame)
- Loss of interest in activities
- Feeling detached or estranged from others
- Inability to experience positive emotions
4. Hyperarousal
The nervous system remains in a permanent state of alert:
- Irritability and outbursts of anger
- Self-destructive or reckless behavior
- Hypervigilance (constantly scanning the environment for danger)
- Exaggerated startle response
- Concentration difficulties
- Sleep problems
Causes of PTSD
Not every person exposed to trauma develops PTSD. Research identifies several factors that influence vulnerability:
- Type of trauma — Interpersonal traumas (assault, abuse) carry higher risk than natural disasters.
- Severity — The more severe, prolonged, or repeated the event, the higher the risk.
- Personal history — Previous traumas, pre-existing mental health issues, or a difficult childhood increase vulnerability.
- Social support — Lack of support after the event or invalidating reactions (“just get over it”) significantly increase risk.
- Biological factors — Genetic predisposition, nervous system sensitivity, and cortisol levels influence the response.
Scientifically Validated Treatment Options
EMDR (Eye Movement Desensitization and Reprocessing)
Developed by Francine Shapiro (2018), EMDR uses bilateral stimulation (eye movements, alternating sounds, or touches) to facilitate processing of traumatic memories. It is recommended as a first-line treatment by the World Health Organization.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
Includes specific techniques such as:
- Prolonged exposure — Gradual and safe confrontation with traumatic memories
- Cognitive processing — Identifying and modifying distorted beliefs related to trauma
- Cognitive restructuring — Developing a more balanced perspective on the event
Somatic Experiencing
Developed by Peter Levine, this approach focuses on releasing energy “trapped” in the body during the traumatic event. It works with bodily sensations rather than verbal narrative.
Medication
In moderate-to-severe cases, medication can be a useful adjunct:
- SSRIs (selective serotonin reuptake inhibitors) — Sertraline and paroxetine are specifically approved for PTSD
- Prazosin — May be useful for PTSD-associated nightmares
- Medication is prescribed by a psychiatrist and works best in combination with psychotherapy
Exercise: The 5-4-3-2-1 Grounding Technique
When you feel overwhelmed by traumatic memories or anxiety, this technique brings you back to the present:
- Name 5 things you can see around you
- Name 4 things you can touch or feel
- Name 3 things you can hear
- Name 2 things you can smell
- Name 1 thing you can taste
Breathe deeply between each step. This technique activates the prefrontal cortex and helps you exit the traumatic response.
When to Seek Professional Help
- Symptoms last more than one month after the traumatic event
- Symptoms are worsening rather than improving
- Functioning at work or in relationships is significantly affected
- You use alcohol or other substances to cope
- You have frequent flashbacks that confuse or frighten you
- You feel disconnected from your life and loved ones
- You have thoughts of self-harm or suicide (contact emergency services immediately)
Conclusion
PTSD is a treatable condition. The research of the past 30 years has produced effective treatments that can significantly reduce symptoms and restore quality of life. The most important thing you can do is not suffer in silence. Healing begins with the courage to ask for help.
PTSD does not mean you are broken. It means something happened to you that exceeded your processing capacity — and that you deserve specialized help to heal.
This article provides educational information and does not replace consultation with a mental health professional. If you are experiencing persistent difficulties, I encourage you to schedule a consultation.